Benefits of a MiniMed Insulin Pump
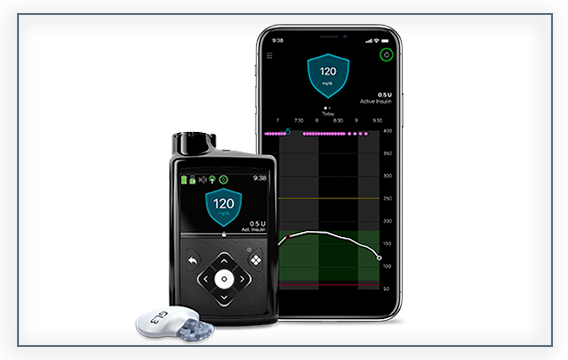
An insulin pump is a small device that mimics the function of your pancreas by providing continuous, customized doses of insulin based on your body’s needs.
Medtronic’s selection of insulin pumps gives you the flexibility to continue living your life while managing your diabetes!

What is Insulin Pump Therapy?
An insulin pump is a small device that mimics the function of your pancreas by providing continuous, customized doses of insulin based on your body’s needs. Insulin pump therapy not only means 90% fewer injections*, but allows for mealtime dosing, more stable blood sugar levels, and accurate insulin delivery!
Not sure how an insulin pump works? Watch the video below!
Why Choose a Medtronic Insulin Pump?
Medtronic has more than 35 years of experience, over 1.2 million people living with diabetes served, and offers service and support to help you succeed with your new insulin pump therapy! Medtronic’s systems include intuitive features that help you manage your diabetes better.
SmartGuard™ Auto Mode
The MiniMed™ 670G system is the only system that automatically adjusts background insulin every five minutes based on your sugar levels.†
Benefits of the SmartGuard™ Auto Mode include:
-
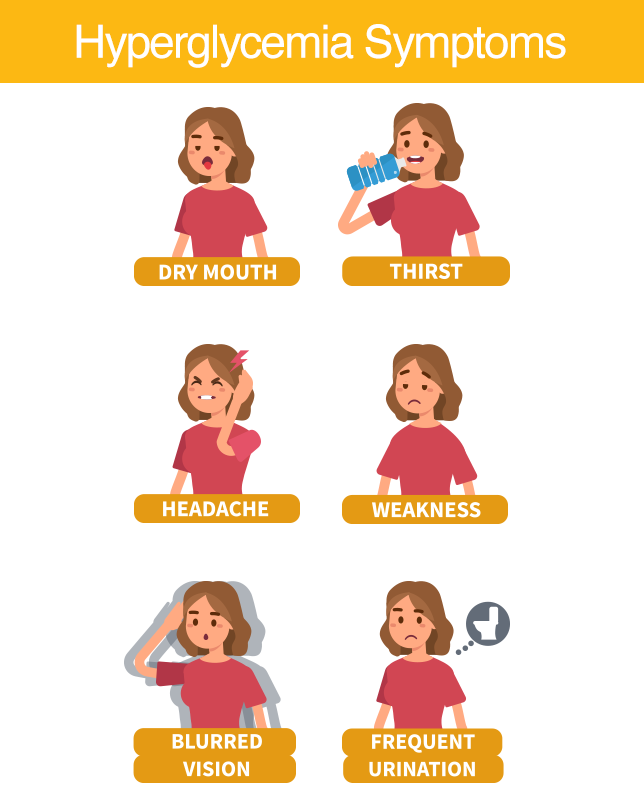
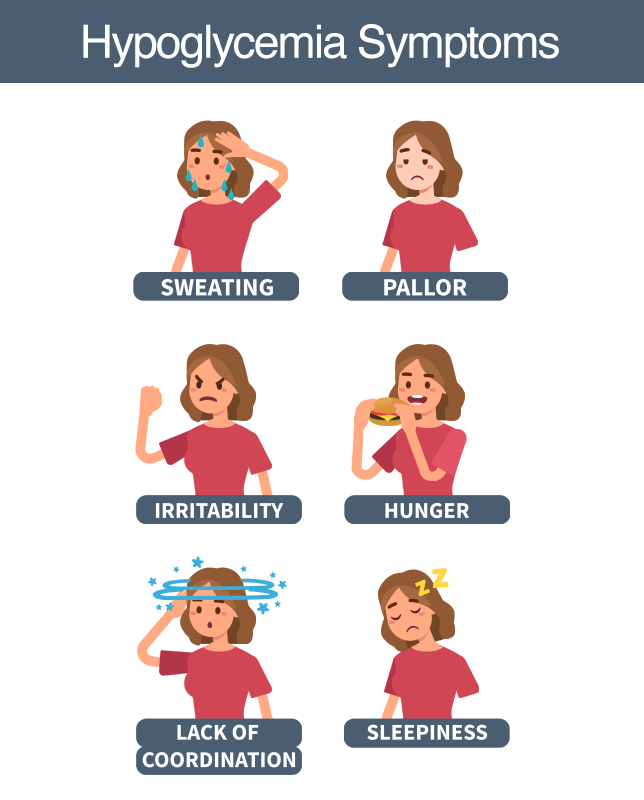
Fewer highs and lows 3
-
Personalized diabetes management 3
-
More freedom to focus on your day 3, 9
-
Less effort to manage diabetes 9

Service and Support
-
24-Hour Technical Support to answer your questions
-
Largest support team consisting of over 2,000 field, clinical and customer care representatives
-
Personalized education and training programs
-
Dedicated insurance service teams to support your insurance needs
Exclusive CareLink™ Software
- A web-based program that collects information directly from your Medtronic diabetes management system. It allows you to generate reports that can be used during your doctor’s visits and to monitor your own progress.
Learn More About Metronic Insulin Pumps
Learn MoreWARNING: Do not use the Suspend on low feature to prevent or treat low glucose. Always confirm your sensor glucose reading using your BG meter, and follow the instructions of your healthcare professional to treat low glucose. Using Suspend on low alone to prevent or treat low glucose may result in prolonged hypoglycemia.
‡ Coverage guidelines for insulin pumps vary and are subject to the insurance companies published medical policies in effect at the time services are requested.
*Assumes four injections per day for 30 days and one infusion set change every two to three days.
† Refers to Auto Mode. Some interaction required. Individual results may vary.
3. Pivotal Trial: Bergenstal R, Garg S, Weinzimer S, et al. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. JAMA. 2016;316(13):1407–1408.
9. Data on file. Survey of Priority Access patients (n>13,000).
This post is sponsored by Medtronic.
Tags: Diabetes, Diabetes Management, Diabetes Supplies, Insulin Pump Therapy, Insulin Pumps, Medtronic